The Plant-Based Community Cookery School
The Plant-Based Community Cookery School
Posted Wednesday 12th October 2016...
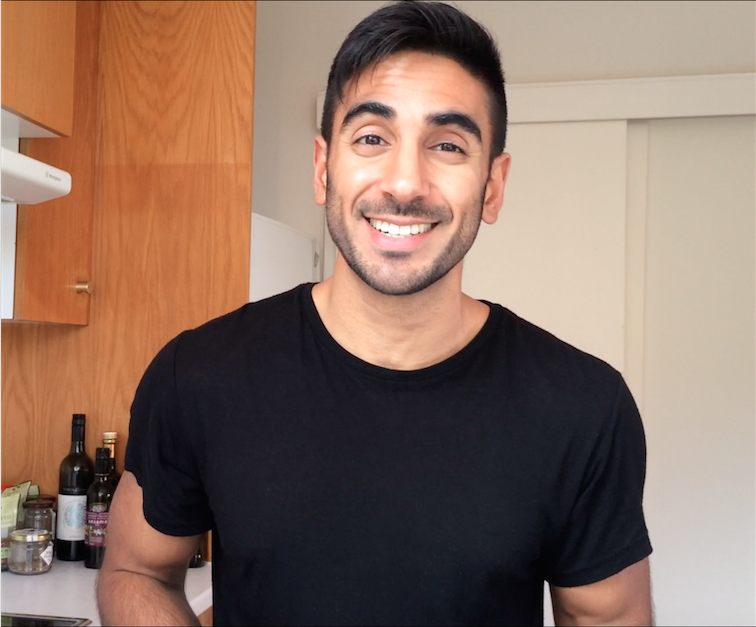
MIH founder Sarah Bentley chats to GP, ‘Doctor’s Kitchen’ blogger and Made in Hackney volunteer Rupy Aujla about how the NHS could be transformed to put food at the center of disease prevention – and save billions of £££ in the process.
Sarah: Let’s get straight to it. So I’ve heard GPs receive very little nutrition training during their medical degree. Is this true?
Rupy: The short answer is yes. The focus isn’t on nutrition in terms of the way a GP’s training is delivered. At med school there’s probably less than 10 hours nutrition training. For a GP we do 2 years of foundation doctor training after medical school. Then specialty training for 3 years which could be in pediatrics, surgery, psychiatry etc. The focus on nutrition is very much dependent on what the importance your Vocational Training Scheme coordinator places on it. You might get a session on nutrition if you’re lucky. But the focus tends to be on training for exams.
Sarah: What’s the consequence of this and how would you remedy the problem?
Rupy: I would make sure all medical students have culinary medical training as a compulsory part of the curriculum. Once you’re able to motivate and inspire students from the foundation level of their training that food is medicinal, that food has an incredibly important effect on disease outcome and prevention - then we’re more likely to see it taken seriously. How medical school is taught differs throughout the country. But you have a set list of specialty subjects, and I want culinary medicine to be one of those.
It’s a complex topic. There’s lots of controversy and debate about what makes an ideal diet. I’m constantly trying to educate my peers and make them aware about all this as no one knows it. There’s the low carbs stance, vegan stance, Mediterranean stance. If you don’t have a foundation in nutrition yourself, how will you answer patients questions about all these different diets that they read about in the media? And the troubling thing is when a patient comes to a GP surgery, they expect GP’s to be fountains of knowledge about everything – and they expect the same thing with nutrition. Now for all manor of reasons - perhaps some GP’s don’t want to feel inferior – in many cases they give out the same outdated advice. All low kcal, low fat – a Weight Watchers diet with all fat stripped out and all that jazz, and it’s just not correct.
Sarah: It’s all very 1980s.
Rupy: Yeah exactly. It’s old information.
Sarah: So what does it take for a patient to be refereed to an NHS dietician?
Rupy: Well sadly the NHS doesn’t hold food in such high regard. Initially they might refer patients to a practice nurse who will in a lot of cases repeat the same outdated NHS advice as the Doctor might be privy too. I’m sure there are some practice nurses who are fantastic, empowered and enthusiastic but this will be because of their own interest and passion about food. To see a dietitian, (something that’s currently quite expensive in the NHS,) patients need to reach a certain peer of unhealthiness. On the cusp of surgery, morbidly obese, that type of thing. But the issue is there are plenty of people with normal physical parameters that still have diabetes bubbling. Many people have pre-diabetes, it’s a huge problem.
There is an army of nutritional therapists willing, but they are not trained to work in and around the NHS framework. But then the area of nutritional therapy is currently quite problematic. There are some smashing ones and some charlatans. It’s difficult as people can call themselves a nutritional therapist after very little training. But then saying that even people that have done a six week course and read up about nutrition as an interest often know much more than Doctors and nurses. They can know a lot more than me – so it’s a bit of a minefield.
Sarah: If you suddenly became head of the NHS tomorrow, what changes would you make to introduce a more preventative, food centered approach to health care?
Rupy: I’d make sure NHS surgeries were able to refer patients to community cooking classes like Made in Hackney. This would work well for patients, giving them a foundation of cooking. We need to do this to both prevent and reverse disease. Plus programmes like this creates community. The only problem with introducing these kinds of changes, from a management point of view, is that the results aren’t always very tangible and can be hard to monitor. The effects and benefits go beyond the political cycle.
I’d also introduce nutritional therapists into the NHS workforce. This might all seem very expensive but if we don’t make these changes the drug bill will only accelerate. We need to get to the root cause of a problem rather than just prescribe a drug for the symptoms. I’d also increase patient appointment time from the current 8-9 minutes to 15-20minutes, and remunerate medical staff properly for this. A happy workforce is an effective workforce.
Sarah: Is the current healthcare system too drug focused?
Rupy: Yes, we’re pharmaceutical focused from when we start in med and nursing school. I mean, pharmacists will always be drug brokers, but even they can be introduced to food and the importance of its effects. But if you look at where we’re coming from in terms of medical school, it’s not surprising prescribing habits are through the roof. And beyond that we’re in a culture of wanting a quick fix from the doctor. There is a patient expectation to prescribe as opposed to suggesting potentially harder but more effective lifestyle changes. It’s interesting if you look at Japan. I have a Japanese colleague who tells me in high school they were taught all about the properties of food and the importance of a nutrient dense diet. In hospitals patients have diets tailored to their particular conditions. It’s just fabulous.
Sarah: What conditions do you feel can be best addressed with dietary changes, that are commonly treated with drugs?
Rupy: All the biggest diseases of today. Obesity, diabetes, high blood pressure, heart disease, stroke. Currently the collective cost is well over half the NHS’s total budget. And that’s a conservative estimate. I recently heard the figure it cost’s the NHS £1m an hour in terms of everything connected to the treatment of diabetes. £1 in every £9 spent is for diabetes. So the most money is spent on the preventable, lifestyle influenced diseases. Shocking isn’t it.
Sarah: What can people do as conscious eaters to urge change within the NHS to encourage a more food focused approach?
Rupy: That’s a really interesting question. One thing would be to support local groups like Made In Hackney. To attend cooking classes, donate money where possible and lobby your local MP’s to support projects teaching the community about the benefits of good food. People could also go direct and voice their opinions to their local GP and ask them to bring it up at the next Clinical Commissioning Group (CCGs) meeting where budgetary decisions are made for each area. You could ask people to email their local GP – and Made In Hackney could even try to give a talk at a local CCG meeting. There’s a great example of a CCG in Calderdale that have taken a more progressive view and allocated a budget to this type of food education.
Sarah: Although we’ve had individual NHS dieticians attend our cookery classes and say they were fantastic and hugely impressed, our plant-based policy might seen a bit radical by some health professionals.
Rupy: People might have a negative view initially but I totally get your approach. You’re putting the vegetables center stage – after all they’re what people need to eat more of but lack the inspiration. I use some animal products in my recipes but the base of my recipes are vegetarian.
Sarah: Myself and a MIH cookery teacher attended the NHS Xpert training course on diabetes. The scientific stuff explaining what diabetes actually was and how it manifested in your body was great, but the information on good dietary choices and how it was presented was terrible. We went on a supermarket tour with a group of diabetic patients and the whole focus was on what people couldn’t eat. Nutrition poor diet and low fat products were recommended, even one’s with artificial sweeteners, and we know how bad a lot of those are for people. We whizzed through the fruit and vegetable section with a mere, “Yeah, you can go mad in this section,” and then we were off to the cheese section for everyone to lament what they couldn’t eat time and time again. Everyone left the tour depressed, uninspired and misinformed. It was such a wasted opportunity.
Rupy: That makes me so sad. That’s why I always focus on celebrating food. The focus should be on the beauty of food and it’s medicinal impact. What you can’t have is important and needs to be covered, but it will never be inspiring. But if you tell people all about the wonderful things food can do for your body – and how to prepare it, then that can change lives. So keep doing what you’re doing. I think Made In Hackney is great and I will do all I can to support it.
Sarah: Thanks Rupy! Lets get a presentation together for a CCG meeting.
Rupy: I’m in. Lets do it.
You can discover all Rupy's inspiring recipes here on his blog www.thedoctorskitchen.com and Instagram
Rupy is leading a Community Cookery class on Sunday 30 October at Made in Hackney.

